Medicare Has Changed - So Should The Way You Should Check Medical Necessity
The Medicare Payment System (OPPS) has changed from Fee for Service to a Prospective Payment System.
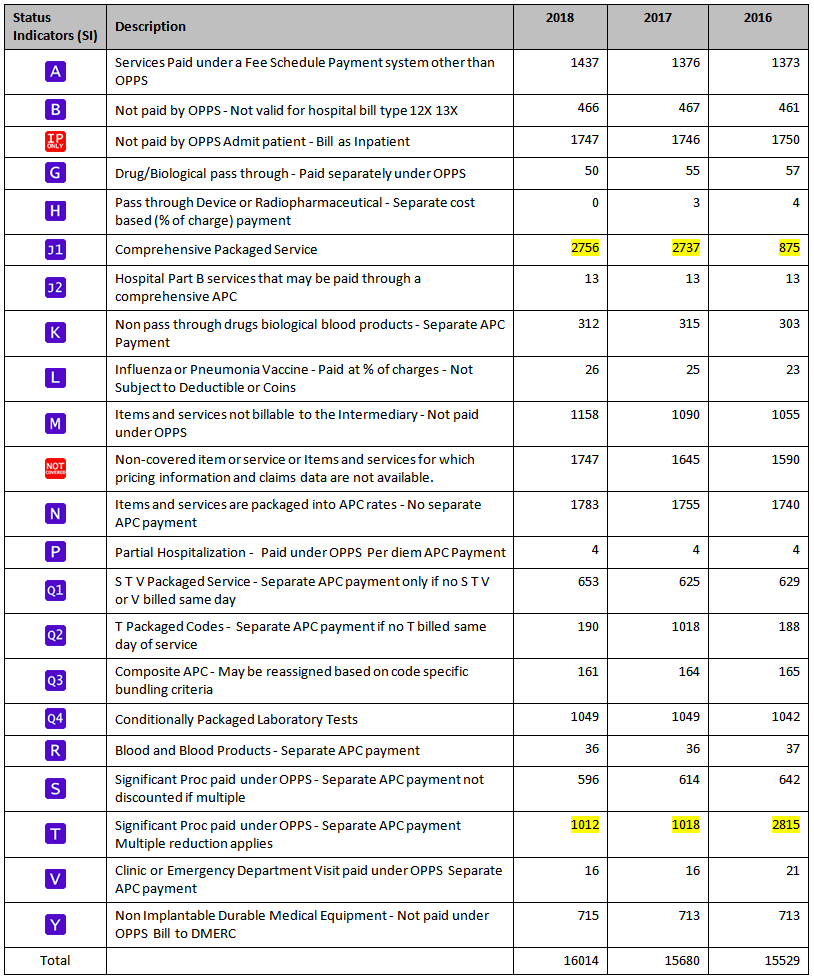
Comprehensive APCs have increased from 875 to 2,737 in just one year. This means the diagnosis must support the J1 Comprehensive APC or the entire claim will be denied with no payment for any of the services that are now part of the "superpackaged" Comprehensive APCs.
- Comprehensive APCs already have an increasing number LCDs and NCDs associated with them.
- A relatively small number of services are exempt from bundling.
- The combination of the Status Indicators on the claim will determine the final payment.
This is why our Medical Necessity solution has the OPPS logic in it's design.
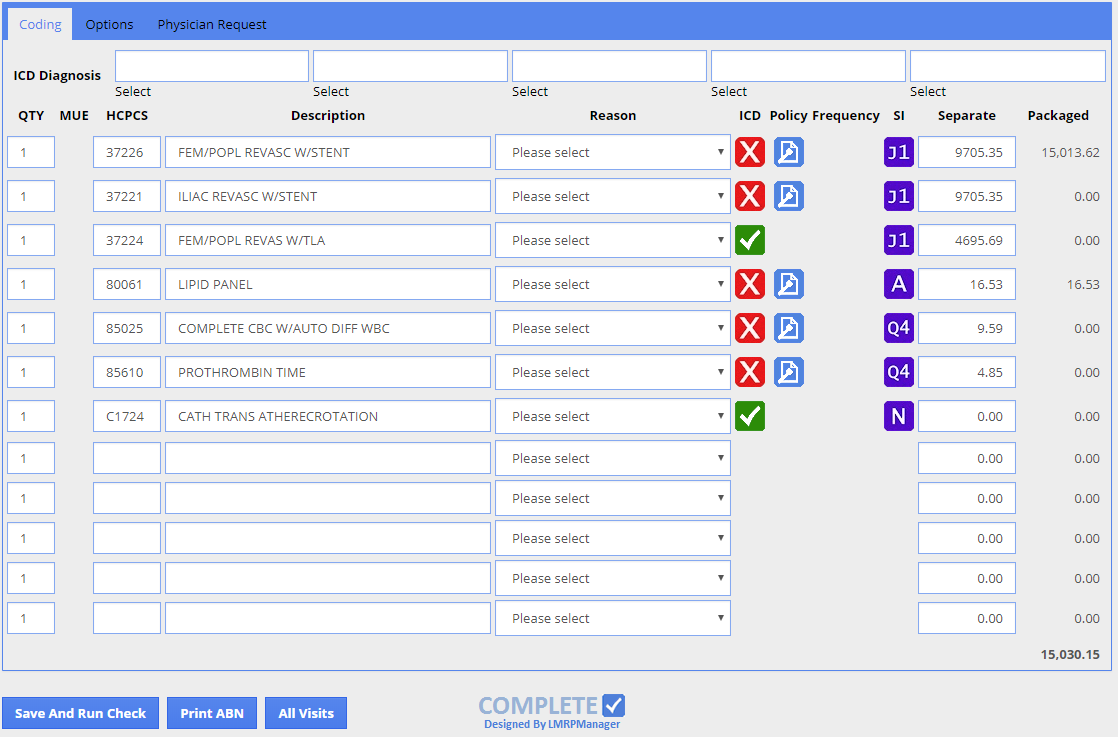
Below is a sample from an actual denied claim. The first HCPCS 37226 is a J1 Comprehensive APC. If it isn't supported, no other services (including the other lower ranked Comprehensive APCs) will be paid. The three J1 Comprehensive APCs in this example also results in a Complexity Adjusted packaged payment of $15,013.62. The value of a Comprehensive APC Denial is much greater because of the way Medicare pays.
As you can see checking the diagnosis vs. individual procedures isn't sufficient when you have a Prospective Payment System.
Comprehensive APCs have increased from 875 to 2,756 from 2016 to 2018.
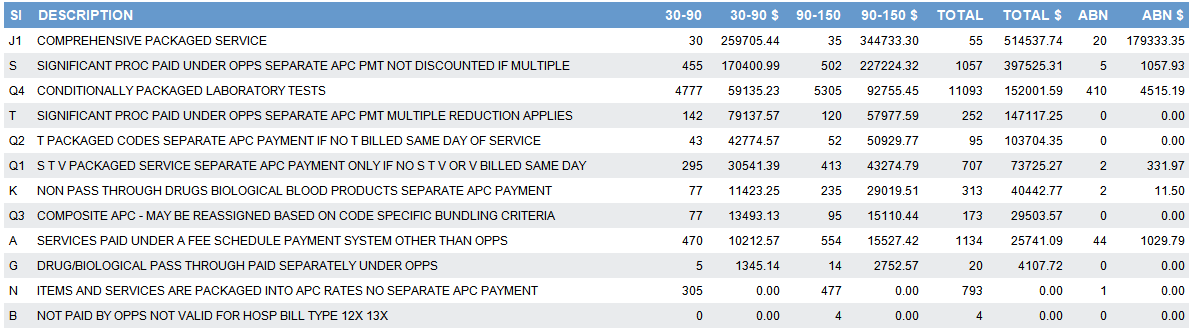
A More Complete Medical Necessity Check Makes Sense Because These Denials are High Dollar and Low Volume