Medical Necessity Solutions Designed for How Medicare Pays Today
 |
Today’s outpatient Medicare payment system is complex and it is changing rapidly. Each year, an increasing number of services that were once paid individually are now packaged into one payment.This unpredictable payment logic leads to larger outpatient denials because packaging places a premium on key procedures. |
|
|
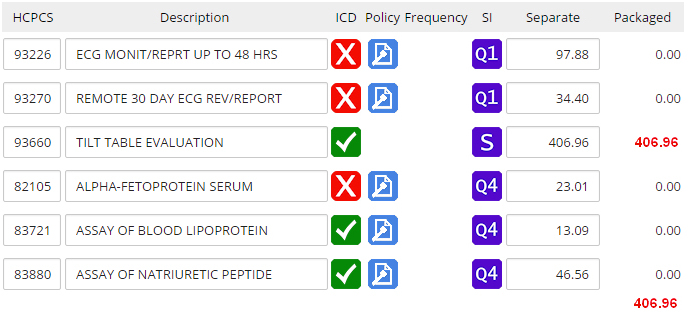
Prospective Payment System Medical Necessity Our solution prevents real denials because it is designed for how Medicare pays today. Our Medicare experts integrated the outpatient payment system into its design so that your staff:
|
|
Sample Information System Screen |
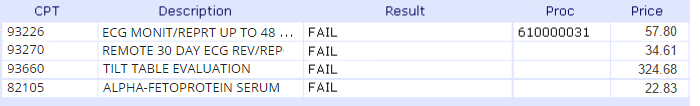
Fee for Service Medical Necessity The medical necessity process on most hospital information systems checks services individually, and without consideration of the packaging logic. This means your staff:
|